T Wave Size Can Predict STEMI Before It Happens
"T waves are the key to life."
Have you ever heard someone say that? 💕
I think they are the most valuable wave we have to tell us about ischemia in the heart.
In order to know what abnormal looks like, we have to have a firm hold on what normal looks like.
So, here are some key tips to know about the T Wave:
🔥 T waves should be upright in all the leads, except for AVR and V1.
🔥 If they were inverted anywhere not in those leads, you have to worry about ischemia.
🔥 "Hyper acute T waves" are T waves that are too big in relation to their QRS complex. (This means early ischemia and STEMI is probably coming)
Can you see the power in this? Detecting early ischemia BEFORE the patient has a STEMI?
This will often show up on the ECG as "non -specific ST T wave changes". So, when it says this really scrutinize you T waves to see if they are "proportianate" to their QRS. If they appear too large they are most likely "hyperacute".
19 year old with palpitations....is it just anxiety?
This 19 year old male presented to the ER feeling like his heart was going to "come out of his chest." He has mild chest pain, mild dyspnea. Denies drug use. VS: 114/90, RR 14, 97.8, 99%. He denies any medical history or medications. This is a tough case, because at first glance this could look regular. And if its not, what is a 19 year old doing with Atrial fibrillation, an "old persons" disease?
His UTOX was negative. His labs including a TSH were all normal. His CXR was normal as well.
His second ECG reveals a clue. He has a delta wave, which is significant for WPW. It is common for young people with WPW to have AF with RVR, and nodal blockers are absolutely not to be used as it will force the electrical impulse down the abberant pathway making the tachycardia worse. His second ECG was done after he was given IV procainamide. He underwent urgent ablation and is doing well.
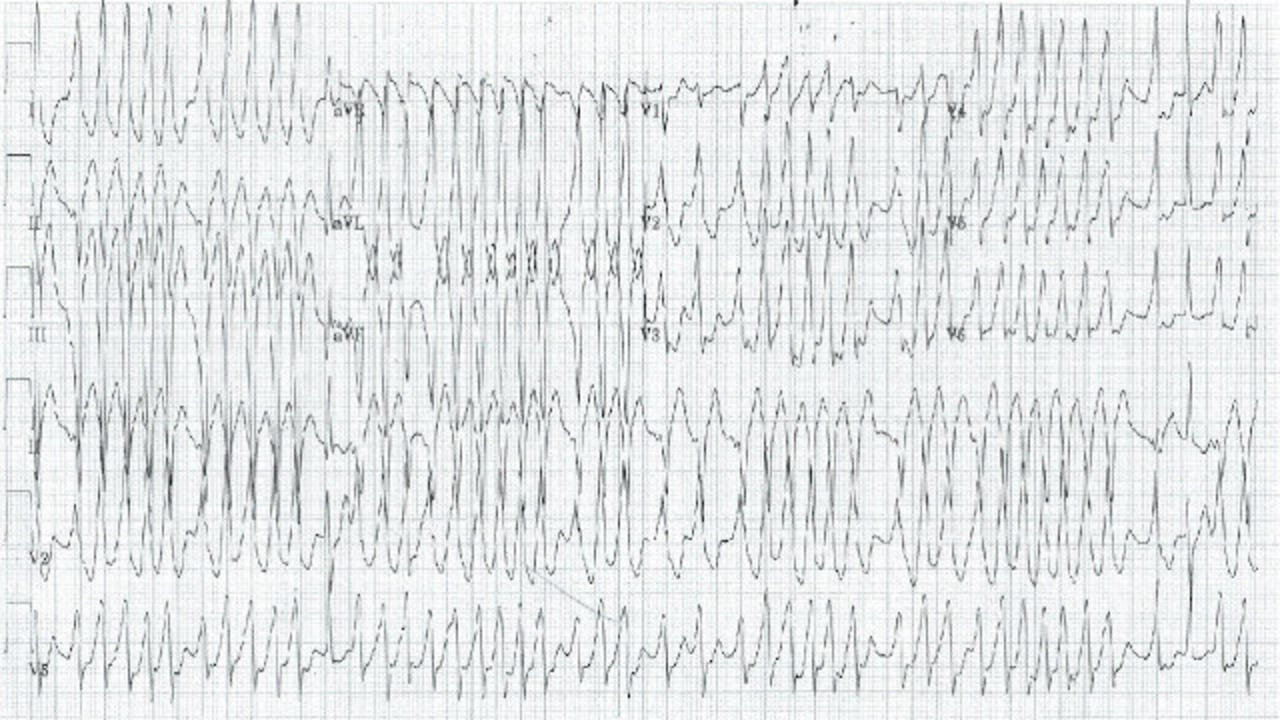
"I watched him have his MI..."
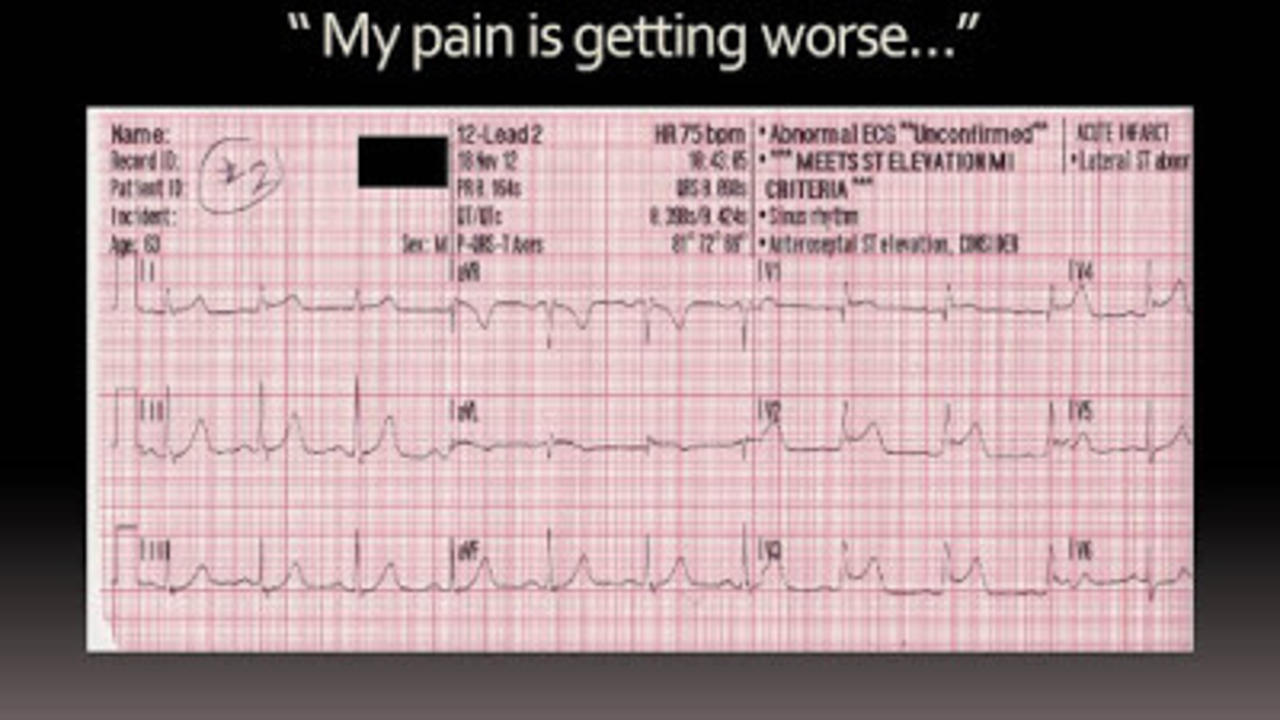
911 responded to a 63 year old male with chest pain. On arrival, the first EKG did not show any ST elevation, and was read as a "normal EKG."
The paramedic reported that 5 minutes later shows the patient having his STEMI. As you can see, he starts to develop a right bundle branch block and completes this is his last EKG.
There is a lot of artifact on that last EKG as the patient was so diaphoretic that the patches would barely stay on.
The patient was taken directly to the cath lab where he was found to have a 99% stenosis of his LAD, his culprit lesion. He ultimately did well although he initially did have a depressed ejection fraction on his echo done post cardiac catheterization.
LAD lesions, (also known as the "Widowmaker") present with ST elevation in V1, V2, V3, and V4 and are often times accompanied by new right bundle branch blocks. You will often see high grade AV blocks as well.
EKG's are just a snapshot in time, and a lot of times can change in minutes. If you are worried ...
